Twelfth Panel Report
The twelfth Citizens' Panel survey was carried out between June 2023 and September 2023.
This report details the findings from the twelfth Panel survey which collected feedback between June 2023 and September 2023. The questions were on two topics:
- organ and tissue donation, and
- the regulation of independent healthcare, which is often called private healthcare.
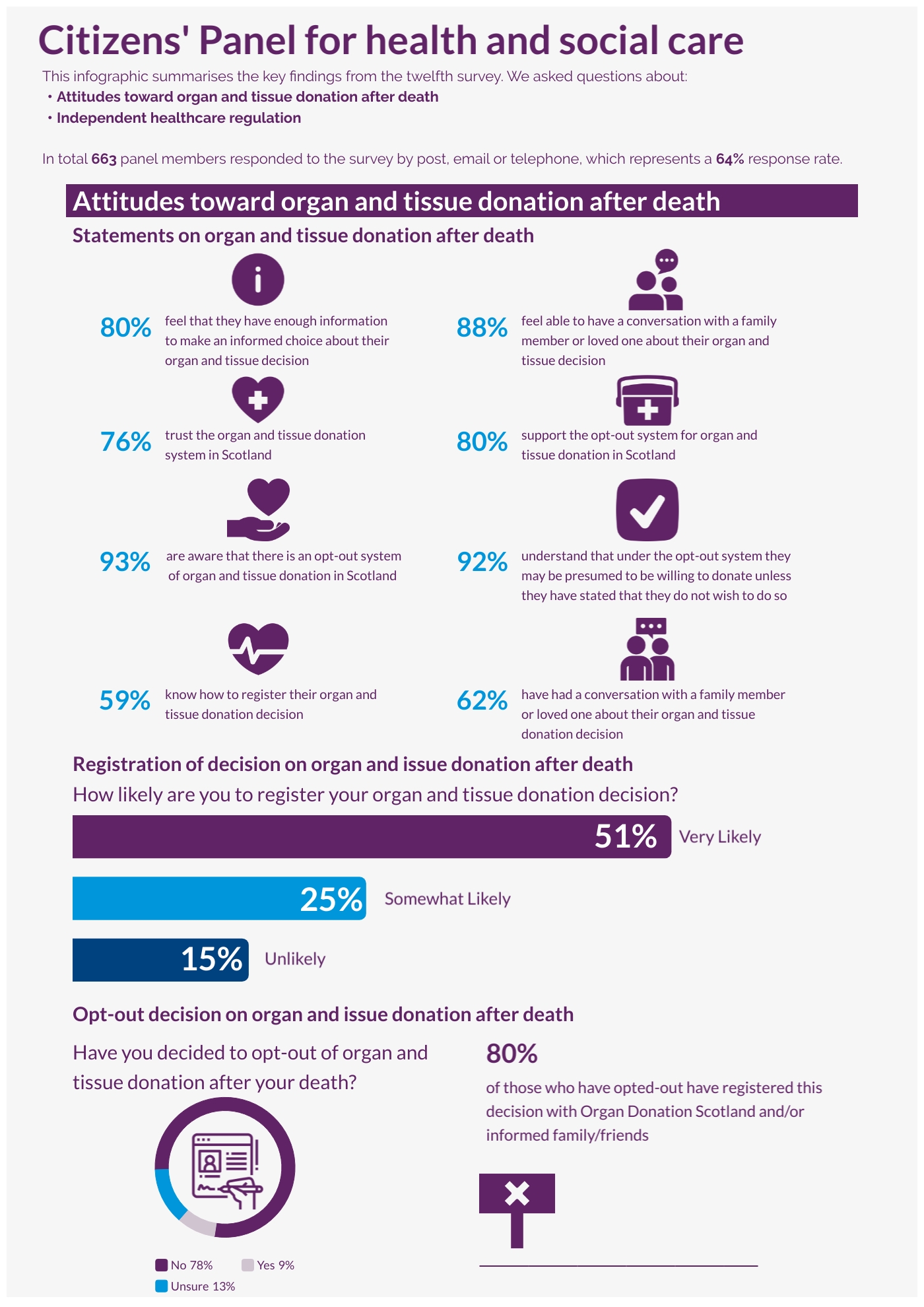
A total of 663 responses (64% response rate) were received, either by post, email or by telephone. This level of return provides data accurate to +/-3.8 % at the overall Panel level. In this report, we do not report results broken down into sub-categories (for example, sex or age) as they are not statistically significant. All comparisons made in this report are statistically significant, unless otherwise stated.
Key findings
Organ and tissue donation
In 2021, Scotland moved to an opt-out system of deceased organ and tissue donation. This means that if someone dies in circumstances where they potentially could become a donor, and they have not registered a donation decision, they would be presumed to be willing to donate, unless their family or friends provide information that the potential donor was unwilling to do so.
Panel members were asked for their opinions on a range of statements about organ and tissue donation after death. The level of agreement ranged from 76% who agreed that they “trust the organ and tissue donation system in Scotland” to 88% who agreed that they “feel able to have a conversation with a family member or loved one about my organ and tissue donation”.
Panel members were asked about their awareness and level of understanding in relation to organ and tissue donation after death:
- 93% were aware that there is an opt-out system for organ and tissue donation in Scotland.
- 92% understood that under the opt-out system they may be presumed to be willing to donate unless they have stated that they do not wish to do so.
- 59% were aware of how to register their organ and tissue donation decision.
More than three quarters of respondents said they were very likely or somewhat likely to register their organ and tissue donation decision (76%). Only 9% of respondents had decided to opt-out of organ and tissue donation after their death and of these individuals (56 respondents), over a third (34%) said they had registered their decision, 18% had informed family or friends of their decision and 28% said they had done both of these things.
The majority of respondents (88%) agreed they feel able to have a conversation with a family member or loved one about their organ and tissue donation decision and more than six in ten respondents (62%) have already had this conversation with a family member or loved one.
Recommendations
Healthcare Improvement Scotland (HIS) recommends that the Scottish Government considers the following when undertaking further awareness campaigns on organ and tissue donation:
- Undertake work on understanding where the pockets of lack of awareness are and how to reach these people.
- Determine how the campaign could increase trust in the system by:
- reporting on the ethics involved and the difference the opt-out system has made to people’s lives, and
- including information about what happens at and after the donation point in campaigns. This should be very clear about how bodies are handled respectfully, which organs and tissue can be donated, and how donations only go to people on the waiting transplant list and are not used for other purposes nor in other contexts.
- Aim to improve information on making an informed choice and highlight misconceptions about who can and cannot donate.
- Continue to raise awareness of organ and tissue donation aspects such as the below, and consider how awareness-raising may achieve wider reach and increased impact:
- how to register a donation decision
- the benefits of registering organ and tissue donation decisions, specifically trying to encourage people who feel they don’t need to register because it is an opt-out system. As in the recommendation above, this should include dispelling misconceptions about who can and cannot donate.
- Focus on marginalised groups, including people with particular faiths and beliefs, and those who are less likely to register.
- Continue to include a call to action in campaigns, such as having a conversation with family and friends regarding people’s organ and tissue donation decision. Consider how this call to action may achieve wider reach and increased impact.
- Integrate the awareness campaign into other processes, where appropriate, such as when giving blood.
The regulation of independent healthcare
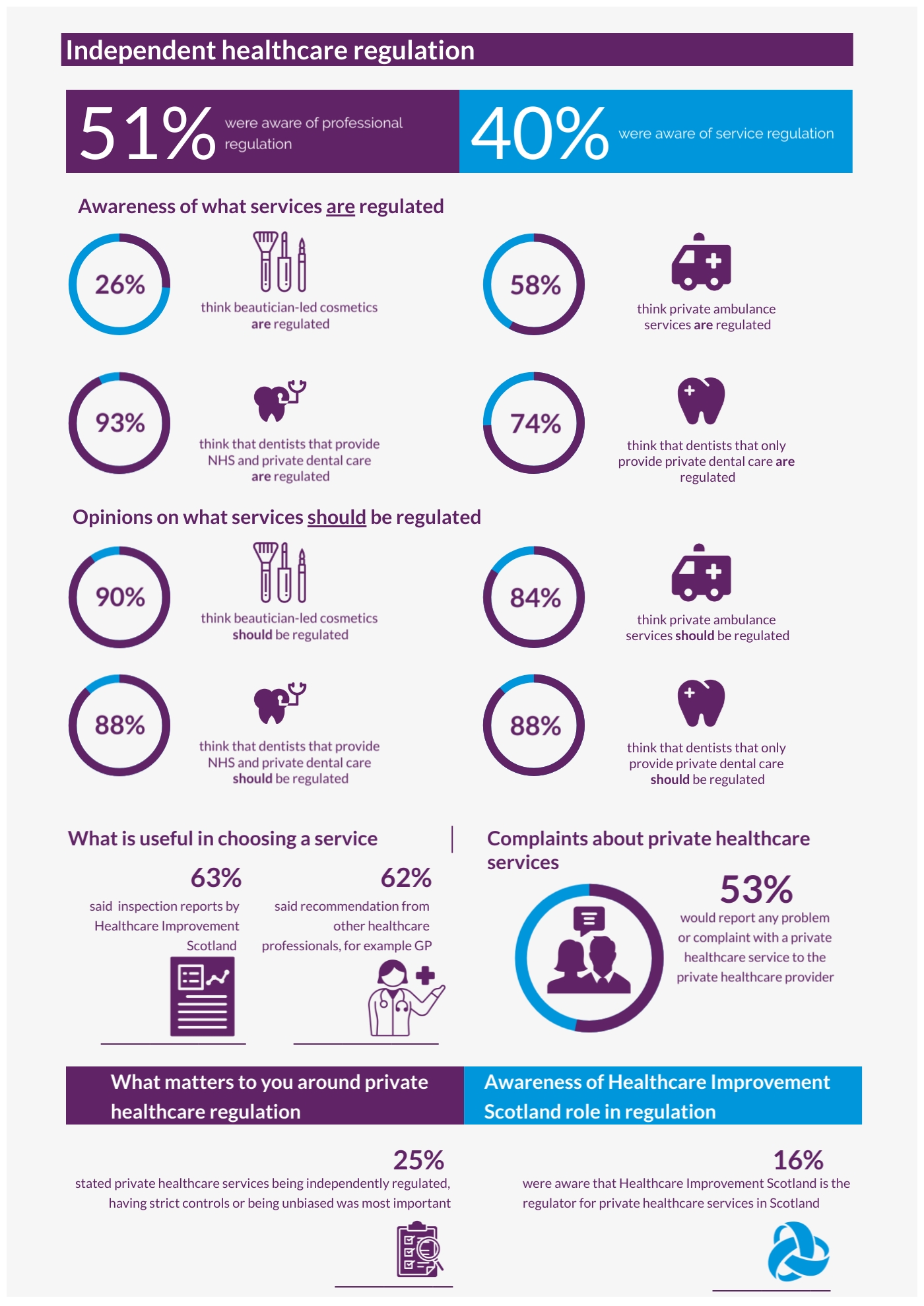
The second half of the questionnaire was on the regulation of independent healthcare, also known as private healthcare services. The aim of this section was to find out the public’s thoughts and awareness about private healthcare and its regulation, to inform future decisions made about the types of treatments and services that will require regulation and any changes required to ensure that regulatory work is helpful and meaningful to the public.
These statutory assurance duties sit with HIS as an organisation and HIS’s Quality Assurance Directorate conducts this regulatory work. This Directorate is separate from HIS’s Community Engagement & Systems Redesign Directorate that carried out the Citizens’ Panel survey.
The private healthcare services that Panel members were most likely to think were regulated were dentists that provide NHS and private dental care (93%), followed by dentists that only provide private dental care (74%). On the other hand, respondents were least likely to think beautician-led cosmetics were regulated (26%). Private ambulance services, beautician-led cosmetics, dentists that provide NHS and private dental care, slimming, nutritional and diet advice provided by dieticians, and internet-based GP and prescription services are not currently regulated. However, Panel members thought that these services are regulated, highlighting misconceptions around the scope of current regulation.
Private healthcare services that Panel members think should be regulated included beautician-led cosmetics (90%), followed by dentists that only provide private dental care (88%), dentists that provide NHS and private dental care (88%), internet-based GP and prescription services which operate only online and don’t have clinics or premises (88%) and nurse or doctor-led cosmetics (87%).
Panel members were asked about their awareness of professional and service regulation. Awareness of these was relatively low, and respondents were more likely to say they were aware of professional regulation (51%) than service regulation (40%).
Over half of respondents said that if they had a problem or complaint about a private healthcare service they would report their concern at first instance to the private healthcare provider (53%). A further 24% said they would report it to an NHS health board and 22% said they would report it to HIS.
Going online or conducting web searches (50%) was the most common way that respondents would look for inspection reports about a private healthcare service.
The information sources that respondents were most likely to find very useful when planning to use a private healthcare service were inspection reports by HIS (63%), followed by recommendations from other healthcare professionals such as GPs (62%).
Panel respondents’ top three priorities as mattering most when thinking about the regulation of private healthcare were:
- Independently regulated/strict controls/unbiased (25%)
- Patient safety (19%)
- Qualified/professional/well-trained staff (11%)
Over three quarters of survey respondents (76%) were unaware that HIS is the regulator for private healthcare services in Scotland.
Recommendations
Based on these findings, we make the following recommendations to HIS, Scottish Government, and delivery partners:
- Looking to the future of independent healthcare regulation, Scottish Government and HIS should consider the scope of regulation and ensure that public stakeholders are included in relevant processes so that public views and needs are met, including considering the current findings. When considering the broadening of regulation, these findings could help decide which areas to prioritise based on public views.
- Work to increase public awareness and understanding around this topic. These activities should use a range of methods and platforms to ensure wide reach and should consider the sources of information mentioned by the Citizens’ Panel as useful when planning and implementing awareness-raising activities. As this work would require significant resource, it could follow a gradual and staged approach, with certain aspects, services, or population groups prioritised. This work should look specifically at:
- the scope of the regulation of private healthcare, what is and what is not regulated and why
- the scope and differences between service regulation and professional regulation. Professional regulators, such as the General Medical Council (GMC), should be approached to be involved with this work
- the complaints process, which aspects of care should be addressed and where. The complaints process needs to be clear on the role and responsibilities of HIS and other organisations. This should also include liaising with health boards to ensure they have the appropriate materials and information and can signpost accordingly. This could also include providing relevant information through NHS Inform
- how and where the public can find regulation reports, and how to use this information to inform their decision-making, and
- what the role of HIS is and what it is not, in terms of independent healthcare regulation.
- Consider doing more engagement to further understand what the public want from regulation, and why people may prioritise some services over others.
- Ensure that search engine optimisation for regulation reports on the HIS website is prioritised as part of website development work.
- Consider making it a condition for services when registering that they signpost to the HIS regulation webpages and reports from their website, potentially using the HIS logo to increase visibility.

